One Big Thing All Women Over 40 Must Know About Their Health
If you are over 40, gaining weight without changing your diet, having brain fog, fatigue, mood swings, or sleep disturbances, I’m here to tell you that while you may be experiencing some of these symptoms as part of hormone fluctuations that happen in the peri/menopause phase, your symptoms may very well be exacerbated by Insulin Resistance.
What is Insulin Resistance?
Insulin resistance is often called pre-diabetes and is one step away from Type 2 Diabetes. It occurs when the body’s cells become less responsive to insulin, a hormone responsible for regulating blood sugar levels. Think of insulin as a key that unlocks the doors of your body’s cells to let sugar (glucose) inside. When you eat, especially foods with carbohydrates, your body converts them to glucose and your blood sugar levels rise. Insulin is produced by your pancreas to help your cells take in this sugar for energy.
Now, insulin resistance is like when those cell doors become a bit rusty or stubborn (which can happen more easily in peri/menopause). In other words, even if insulin is knocking on the cell door, it doesn’t open easily. So, your body has to make extra insulin to get the same amount of sugar inside the cells. This leads to an elevation in insulin and blood sugar levels, triggering a cascade of adverse effects on the body.
When your body has to produce extra insulin to compensate for this resistance, it can eventually lead to high levels of insulin in your blood, and that can cause health problems like type 2 diabetes. So, it’s important to maintain a healthy lifestyle with a balanced diet and regular exercise to keep those cell doors working smoothly.
Who is at Risk?
It is estimated that almost one in every two Americans is either Insulin Resistant or Type 2 Diabetic. Many don’t even know they are dealing with this. As a health coach, I was surprised when I learned I had slipped into the realm of insulin resistance.
While Insulin Resistance can happen at any age for men and women, research has shown a significant association between perimenopause and insulin resistance. Estrogen aids in maintaining healthy glucose metabolism by enhancing insulin sensitivity and promoting the efficient utilization of glucose. As estrogen levels decline during perimenopause, insulin sensitivity is compromised, leading to an impaired ability to regulate blood sugar levels effectively. And this is one way women may suddenly gain weight without having changed their diet. In other words, we can’t handle carbohydrates the way we used to.
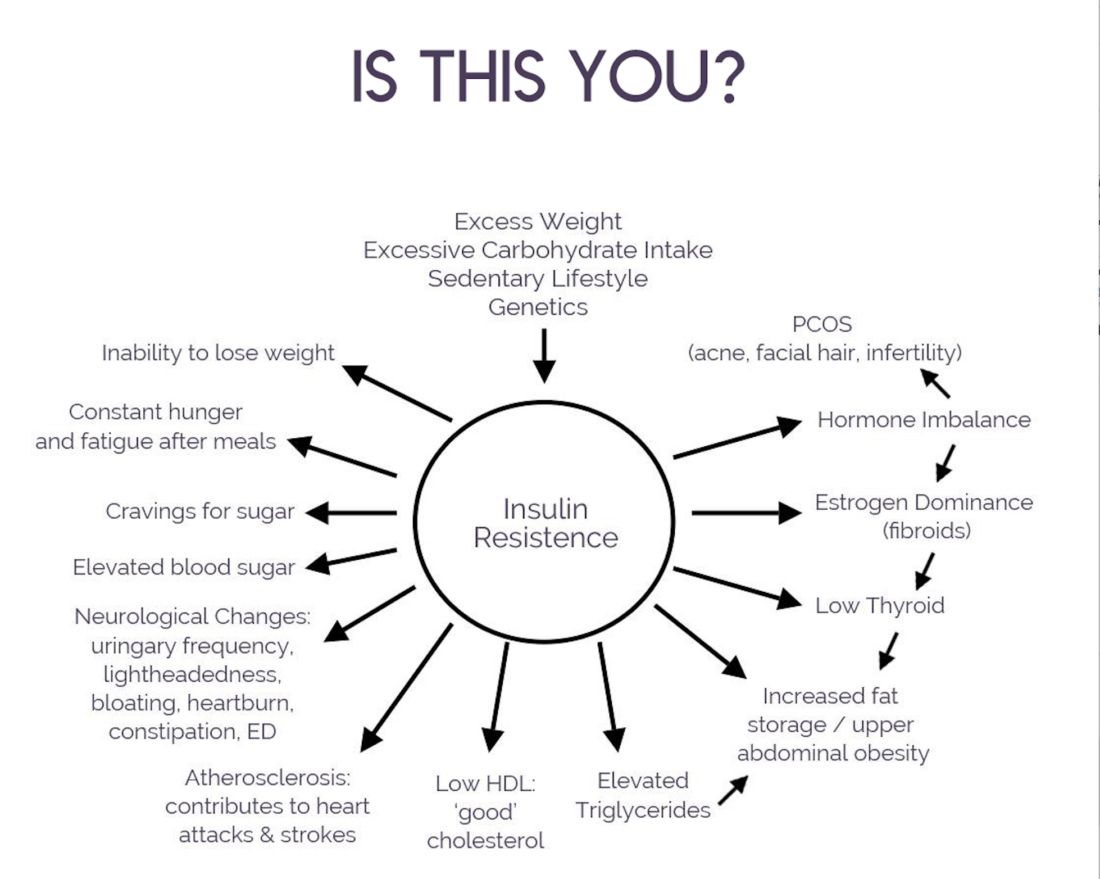
Signs and symptoms of Insulin Resistance:
Spotting the signs of insulin resistance during perimenopause is crucial for early intervention.
Weight Gain: Insulin resistance can contribute to unexplained weight gain, particularly in the abdominal area.
Fatigue and Energy Fluctuations: Insulin resistance can disrupt the body’s energy balance, leading to fatigue or inconsistent energy levels throughout the day.
Mood Swings and Irritability: Insulin resistance may trigger hormonal imbalances, which can manifest as mood swings, irritability, and anxiety when you don’t eat for some time. Hangry anyone?!
Irregular Menstrual Cycles: Perimenopause already brings irregular periods, but insulin resistance can exacerbate these changes.
High cholesterol: in particular triglycerides over 100
Elevated HbA1c – always ask for this marker on your routine physical. You optimally want to be far away from this pre-diabetes cliff so <5.3.
Constant Sugar or Carb Cravings: When glucose can’t get into the cells, the body craves more fast fuel
Darkened Skin Patches on neck and or armpits (called Acanthosis Nigricans)
Why Should You Care? Understanding the impact of insulin resistance on perimenopause is crucial for several reasons:
Quality of Life: By addressing insulin resistance, women may experience a reduction in perimenopause symptoms, leading to an improved quality of life.
Long-Term Health: Insulin resistance is a precursor to inflammatory conditions such as type 2 diabetes, cardiovascular diseases, cancer, dementia and metabolic disorders. Early intervention can mitigate these risks.
Personalized Treatment: Recognizing the link between perimenopause and insulin resistance allows for tailored treatment plans that focus on restoring insulin sensitivity and hormonal balance.
How to Prevent and or Reverse Insulin Resistance
The good news is that you can lower your risk of insulin resistance, and even reverse it through your diet and lifestyle.
Balance blood sugar through diet:
Reduce consumption of refined carbohydrates, sugar, and alcohol
Increase intake of vegetables, protein, and healthy fats, following a Low Glycemic Load (GL) diet
Minimize snacking and focusing on 2 or 3 main meals per day
Explore overnight fasting as an option
Lifestyle Strategies for Managing Stress:
Even if you’re on the best blood sugar balancing diet in the world, you can still be at risk of insulin resistance! That’s because stress can cause it on its own.
In response to stress, the adrenal glands prepare you for the fight or flight response by putting sugar into the blood and thereby raising your blood sugar levels. In addition, high cortisol levels can prevent insulin from doing its job of transporting glucose into cells which forces the body to store it as fat.
Prioritize self-care and stress management to regulate stress hormones, which is crucial for maintaining stable blood sugar levels.
Incorporate exercise:
Stay physically active, but avoid excessive exercise. Strength training helps maintain muscle mass, which aids in glucose storage and minimizes insulin production.
Get adequate sleep:
Align with your daily Circadian rhythm for healthy insulin management. Prioritize sleep, receive daylight exposure upon waking, and wind down at night, avoiding electronic devices and artificial lighting. This helps your body produce the appropriate hormones, including serotonin and melatonin.
Monitor your health:
Start by checking your HbA1c levels, which your doctor can assess. Other potential tests include fasting insulin levels or glucose tolerance tests. If you want to monitor how your diet and lifestyle impact your blood sugar levels, you can try a continuous glucose monitor for a 14-day trial.
If you are not sure where to start and would like guidance and accountability, consider my upcoming 21-Day Reset as a great place to start! Here we share tips and tricks on not only how to manage blood sugar, but how to gradually phase out less healthy food and replace old habits with new habits that support your health goals. We guide you every step of the way and would love for you to join us! To learn more, head on over to my website.
Yours in health,
Linda
References:
Lovejoy JC, et al. (2008). Increased visceral fat and decreased energy expenditure during the menopausal transition. International Journal of Obesity, 32(6), 949-58.
Shifren JL, et al. (2010). Role of Hormones in the Etiology and Treatment of Menopausal Insulin Resistance. The Journal of Clinical Endocrinology & Metabolism, 95(7), 2843-2850.
Golden SH, et al. (2007). Endogenous sex hormones and glucose tolerance status in postmenopausal women. The Journal of Clinical Endocrinology & Metabolism, 92(4), 1289-1295.